- Volumes 84-95 (2024)
-
Volumes 72-83 (2023)
-
Volume 83
Pages 1-258 (December 2023)
-
Volume 82
Pages 1-204 (November 2023)
-
Volume 81
Pages 1-188 (October 2023)
-
Volume 80
Pages 1-202 (September 2023)
-
Volume 79
Pages 1-172 (August 2023)
-
Volume 78
Pages 1-146 (July 2023)
-
Volume 77
Pages 1-152 (June 2023)
-
Volume 76
Pages 1-176 (May 2023)
-
Volume 75
Pages 1-228 (April 2023)
-
Volume 74
Pages 1-200 (March 2023)
-
Volume 73
Pages 1-138 (February 2023)
-
Volume 72
Pages 1-144 (January 2023)
-
Volume 83
-
Volumes 60-71 (2022)
-
Volume 71
Pages 1-108 (December 2022)
-
Volume 70
Pages 1-106 (November 2022)
-
Volume 69
Pages 1-122 (October 2022)
-
Volume 68
Pages 1-124 (September 2022)
-
Volume 67
Pages 1-102 (August 2022)
-
Volume 66
Pages 1-112 (July 2022)
-
Volume 65
Pages 1-138 (June 2022)
-
Volume 64
Pages 1-186 (May 2022)
-
Volume 63
Pages 1-124 (April 2022)
-
Volume 62
Pages 1-104 (March 2022)
-
Volume 61
Pages 1-120 (February 2022)
-
Volume 60
Pages 1-124 (January 2022)
-
Volume 71
- Volumes 54-59 (2021)
- Volumes 48-53 (2020)
- Volumes 42-47 (2019)
- Volumes 36-41 (2018)
- Volumes 30-35 (2017)
- Volumes 24-29 (2016)
- Volumes 18-23 (2015)
- Volumes 12-17 (2014)
- Volume 11 (2013)
- Volume 10 (2012)
- Volume 9 (2011)
- Volume 8 (2010)
- Volume 7 (2009)
- Volume 6 (2008)
- Volume 5 (2007)
- Volume 4 (2006)
- Volume 3 (2005)
- Volume 2 (2004)
- Volume 1 (2003)
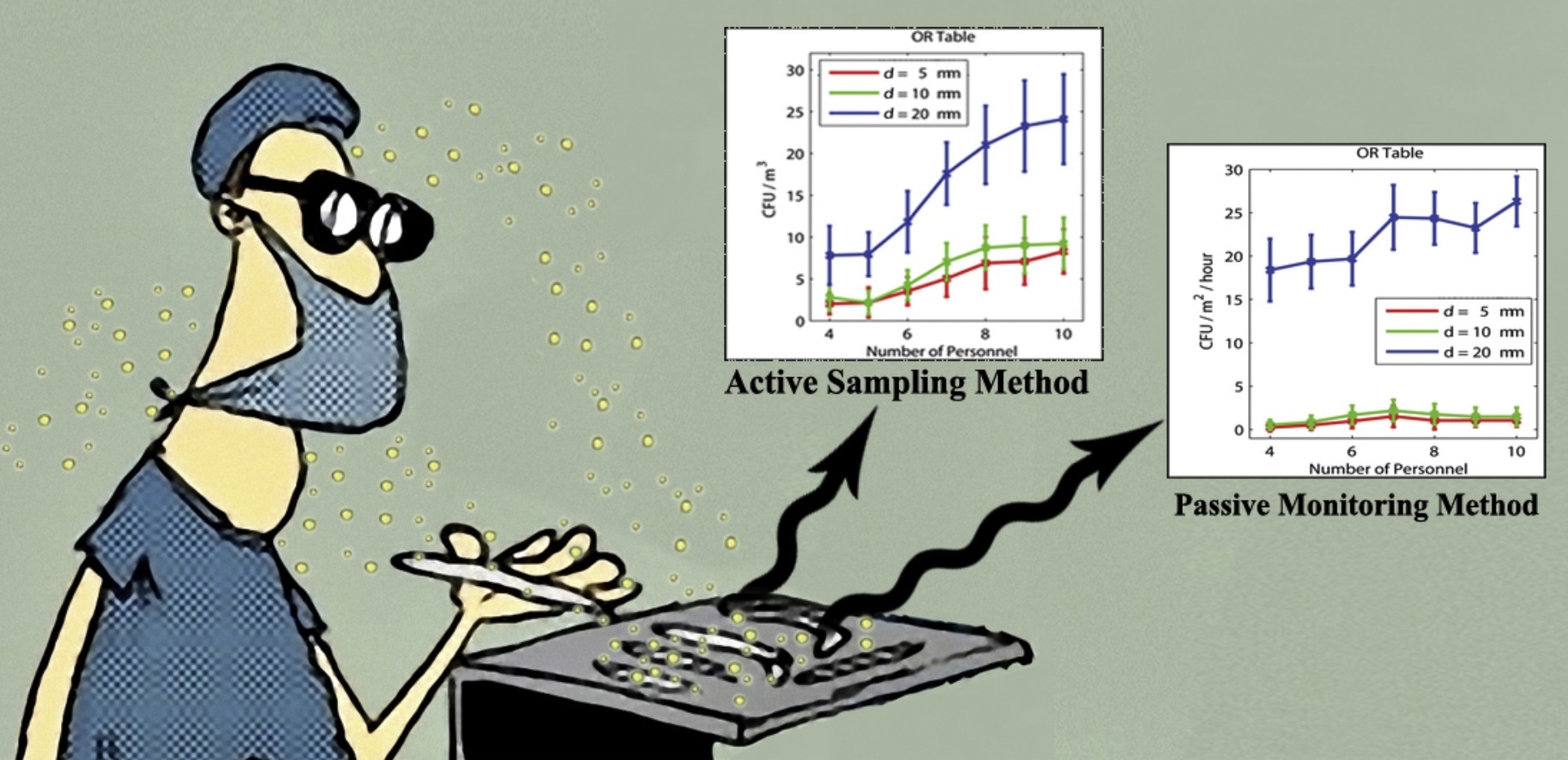
• Two staff member configurations were modeled in the operating room (OR).
• Both active sampling and passive monitoring approaches were examined numerically.
• Increasing personnel number increases the bacteria-carrying particles in the OR.
• The growing rates highly depend of the staff constellation.
• Active sampling method reveals more predictable results compared to passive monitoring method.
Prediction of bacteria-carrying particle (BCP) dispersion and particle distribution released from staff members in an operating room (OR) is very important for creating and sustaining a safe indoor environment. Postoperative wound infections cause significant morbidity and mortality, and contribute to increased hospitalization time. Increasing the number of personnel within the OR disrupts the ventilation airflow pattern and causes enhanced contamination risk in the area of an open wound. Whether the amount of staff within the OR influences the BCP distribution in the surgical zone has rarely been investigated. This study was conducted to explore the influence of the number of personnel in the OR on the airflow field and the BCP distribution. This was performed by applying a numerical calculation to map the airflow field and Lagrangian particle tracking (LPT) for the BCP phase. The results are reported both for active sampling and passive monitoring approaches. Not surprisingly, a growing trend in the BCP concentration (cfu/m3) was observed as the amount of staff in the OR increased. Passive sampling shows unpredictable results due to the sedimentation rate, especially for small particles (5–10 μm). Risk factors for surgical site infections (SSIs) must be well understood to develop more effective prevention programs.
Air quality; Surgical site infection; Airborne particle control; Hospital operating room; Ventilation system
